The contribution of medical physicists in Radiation Oncology department in the Royal Hospital during COVID-19 can be summarized as follows. The Radiation Oncology physicist team was divided into two groups alternated every three days, so that every day of the week there was only one group (three physicists) in the department. This was a measure taken to reduce the possibility of spreading the infection among the two groups and for having always a backup team ready to support the RT services in case of need or any emergency, so that the service would not be interrupted. The most urgent work for the medical physicists supporting Radiation Oncology department is the RT treatment planning, second dose checks, patient-specific treatment QA and weekly machine QA. There was a trial for the remote connection to treatment planning workstations so that the physicists could work from home.
The Quality Control tests were done routinely, whereas the acceptance checks for new devices (not commenced with clinical service) have been postponed, except the acceptance tests for the new HDR source.
There were remote discussions among radiation medical physicists, that were held twice a week, to discuss new planned cases and other issues related to the patient-specific QA and machine QAs, and to solve questions regarding the medical physics part. Moreover, during the pandemic, most of the physicists found the opportunity to improve and update their knowledge and skills via attending webinars and virtual training and courses.
Regarding health physics, the personal TLD monitoring period was extended to two months instead of one month. Additionally, for any suspected or infected staff, his/her TLD badge was kept in a separate envelope and the Radiation Protection Service had to be informed.
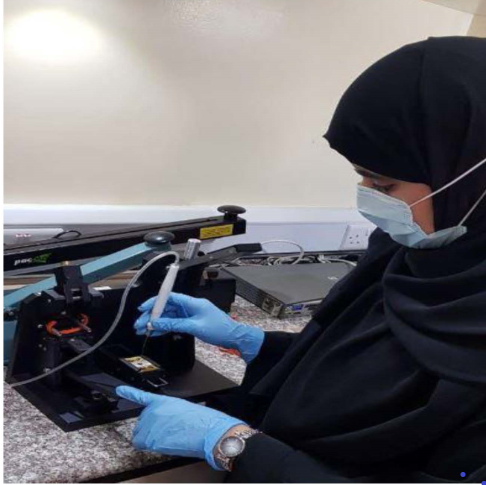
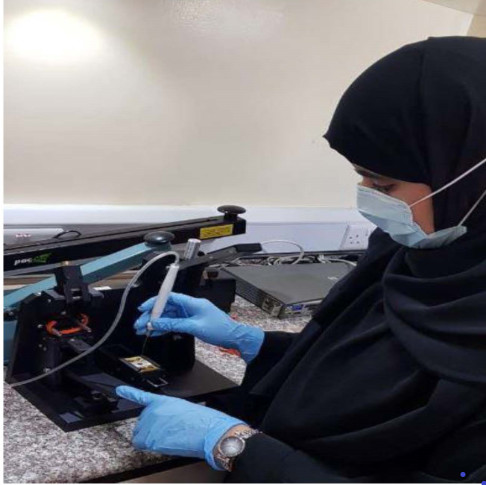
During the normal hours work, the Radiation Oncology physicists were taking optimal precautions to reduce the possibility of being infected or spreading COVID-19 via wearing the face mask and avoiding going to crowded places, like the treatment waiting area. They were regularly and thoroughly cleaning their hands with an alcohol-based hand rub (there was at least one in each treatment planning room) or wash with soap and water. Moreover, the physicists maintained at least 2 meters distance between themselves, by locating treatment planning workstations at a distance larger than 2 m. Generally, this period was a good opportunity to update the QC checks and workflow protocols and policy documents.
Zakiya AL Rahbi, Ph. D
Sr. Specialist Medical Physicist (A)
Radiation Protection Supervisor
Radiation Oncology, National Oncology Center
The Royal Hospital, Muscat
Sultanate of Oman
The Quality Control tests were done routinely, whereas the acceptance checks for new devices (not commenced with clinical service) have been postponed, except the acceptance tests for the new HDR source.
There were remote discussions among radiation medical physicists, that were held twice a week, to discuss new planned cases and other issues related to the patient-specific QA and machine QAs, and to solve questions regarding the medical physics part. Moreover, during the pandemic, most of the physicists found the opportunity to improve and update their knowledge and skills via attending webinars and virtual training and courses.
Regarding health physics, the personal TLD monitoring period was extended to two months instead of one month. Additionally, for any suspected or infected staff, his/her TLD badge was kept in a separate envelope and the Radiation Protection Service had to be informed.
During the normal hours work, the Radiation Oncology physicists were taking optimal precautions to reduce the possibility of being infected or spreading COVID-19 via wearing the face mask and avoiding going to crowded places, like the treatment waiting area. They were regularly and thoroughly cleaning their hands with an alcohol-based hand rub (there was at least one in each treatment planning room) or wash with soap and water. Moreover, the physicists maintained at least 2 meters distance between themselves, by locating treatment planning workstations at a distance larger than 2 m. Generally, this period was a good opportunity to update the QC checks and workflow protocols and policy documents.
Zakiya AL Rahbi, Ph. D
Sr. Specialist Medical Physicist (A)
Radiation Protection Supervisor
Radiation Oncology, National Oncology Center
The Royal Hospital, Muscat
Sultanate of Oman




 Officers
Officers